Immunotherapy has emerged as a groundbreaking approach in cancer treatment, harnessing the body’s immune system to fight cancer cells. Unlike traditional therapies, which often damage healthy tissues, immunotherapy offers a more targeted and potentially effective treatment strategy. This article explores the significant advancements in immunotherapy, including checkpoint inhibitors, CAR T-cell therapy, and cancer vaccines. It also addresses the challenges associated with immunotherapy, such as high costs, variable patient responses, and potential side effects. By understanding these innovations and limitations, patients and healthcare providers can better navigate the evolving landscape of cancer care.
Introduction
Cancer continues to be one of the leading causes of death worldwide, with millions of people affected each year (American Cancer Society, 2024). Traditional treatments, including surgery, chemotherapy, and radiation therapy, have contributed to saving lives but often come with significant limitations, such as toxicity and severe side effects. Moreover, these treatments are not always effective for advanced or metastatic cancers (Ribas & Wolchok, 2018). In recent years, immunotherapy has emerged as a promising treatment option that leverages the body’s immune system to target and destroy cancer cells. Immunotherapy, unlike conventional treatments, uses the body’s natural defenses, which can lead to more targeted and long-lasting effects (Sharma & Allison, 2015).
Breakthroughs in Immunotherapy
1. Checkpoint Inhibitors Unleashing the Immune System: Checkpoint inhibitors represent one of the most significant advancements in immunotherapy. These drugs target immune checkpoint proteins, such as PD-1 and CTLA-4, which act as “brakes” on the immune system. In a healthy immune response, these checkpoints help prevent the immune system from attacking normal cells. However, cancer cells can exploit these checkpoints to evade detection and destruction (Topalian, Drake, & Pardoll, 2015). Checkpoint inhibitors, such as pembrolizumab (Keytruda®) and nivolumab (Opdivo®), block these checkpoint proteins, effectively “releasing the brakes” and enabling immune cells, particularly T-cells, to recognize and attack cancer cells (Ribas & Wolchok, 2018).
Clinical trials have shown that checkpoint inhibitors can significantly improve survival rates for patients with advanced melanoma, non-small cell lung cancer, and Hodgkin’s lymphoma (Ribas & Wolchok, 2018). Combination therapies, such as combining a CTLA-4 inhibitor (ipilimumab) with a PD-1 inhibitor, have also demonstrated enhanced effectiveness, though these therapies can increase the risk of side effects, including fatigue and skin rashes (Sharma & Allison, 2015).
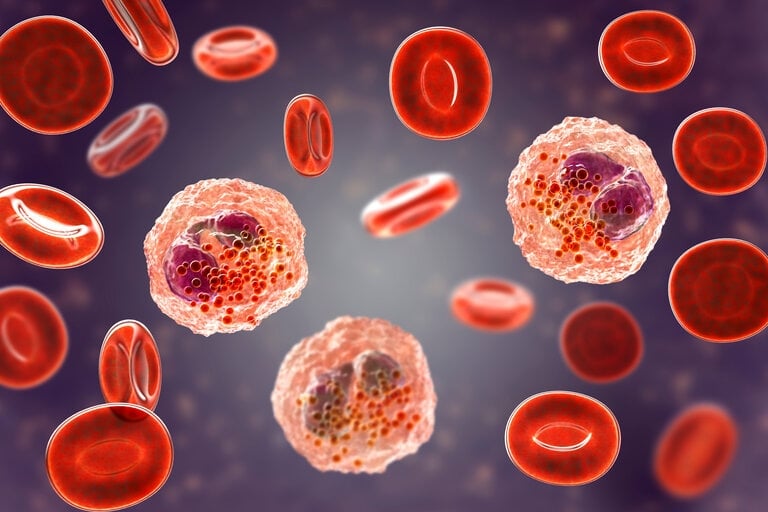
2. CAR T-Cell Therapy: Chimeric Antigen Receptor T-cell (CAR T-cell) therapy is another revolutionary treatment that involves modifying a patient’s own immune cells to target cancer more effectively. T-cells are extracted from the patient’s blood, genetically engineered to produce chimeric antigen receptors (CARs), and then infused back into the patient’s bloodstream (June et al., 2018). These engineered cells can specifically recognize cancer cells by targeting unique proteins on their surface, allowing for more precise and effective targeting.
CAR T-cell therapy has shown outstanding results in treating blood cancers like leukemia and lymphoma, particularly in pediatric patients with acute lymphoblastic leukemia (ALL), where remission rates have reached as high as 83% (Maude et al., 2018). However, the therapy is complex and costly, often exceeding $500,000 per patient (June et al., 2018). Additionally, side effects such as cytokine release syndrome (CRS), which causes a severe inflammatory response, can be life-threatening and require close monitoring and intervention (Rosenberg & Restifo, 2015).
3. Cancer Vaccines and Oncolytic Viruses: Cancer vaccines are another innovative approach to treating cancer. These vaccines come in two forms: preventive and therapeutic. Preventive vaccines, such as the human papillomavirus (HPV) vaccine, have been effective in preventing cancer by protecting against viruses that can cause cancer, such as HPV-related cervical cancer (Schreiber, Old, & Smyth, 2011). Therapeutic vaccines, on the other hand, are designed to treat existing cancers by stimulating the immune system to target and destroy cancer cells. Sipuleucel-T (Provenge®), for example, is used to treat advanced prostate cancer by training the immune system to target prostate cancer cells, extending survival by several months (Farkona, Diamandis, & Blasutig, 2016).
Oncolytic viruses represent another promising strategy in cancer therapy. These are modified viruses that can infect and kill cancer cells while sparing healthy tissue. For instance, T-VEC (Imlygic®), a herpesvirus engineered to target melanoma cells, not only kills tumors directly but also stimulates an immune response that helps attack residual cancer cells (Sharma & Allison, 2015). This dual action of tumor destruction and immune activation offers exciting prospects for treating hard-to-target cancers.
4. Combination Therapies Synergizing Treatments: Combination therapies, which involve using immunotherapy alongside traditional treatments like chemotherapy or radiation, have shown great promise. These combined approaches enhance the immune system’s ability to recognize and destroy tumors. In lung cancer patients, combining checkpoint inhibitors with chemotherapy has resulted in survival rates that are 50% higher than chemotherapy alone (Topalian et al., 2015). Additionally, researchers are investigating combinations of immunotherapy with targeted therapies that focus on specific genetic mutations within cancer cells, offering the potential for even more effective treatments.
Challenges in Immunotherapy
1. High Costs and Limited Accessibility: One of the biggest challenges facing immunotherapy is its high cost. CAR T-cell therapies can exceed $500,000 per treatment, while checkpoint inhibitors can cost over $100,000 annually (June et al., 2018). These high prices limit access to immunotherapy, particularly in low-income countries where healthcare infrastructure may be insufficient. Additionally, CAR T-cell therapies require specialized facilities for manufacturing, further restricting availability (Farkona et al., 2016). Reducing these costs and ensuring more equitable access to these treatments will be critical in making immunotherapy a viable option for a broader patient population.
2. Variable Patient Responses: Immunotherapy does not work equally for all patients. Response rates for checkpoint inhibitors, for example, vary depending on the type of cancer and individual patient factors. Tumors with high levels of PD-L1, a protein that suppresses immune activity, tend to respond better to these treatments (Sharma & Allison, 2015). However, many patients experience little or no benefit, highlighting the need for predictive biomarkers that can help identify which patients are most likely to respond to immunotherapy (Ribas & Wolchok, 2018).
3. Side Effects and Safety Concerns: While immunotherapy has fewer side effects than traditional treatments like chemotherapy, it can still cause serious adverse reactions. Overactivation of the immune system can lead to inflammation in healthy organs, causing conditions such as pneumonitis (lung inflammation) and colitis (colon inflammation) (Topalian et al., 2015). Additionally, CAR T-cell therapy is associated with cytokine release syndrome (CRS), a potentially life-threatening complication (June et al., 2018). Managing these side effects requires close monitoring and the use of medications such as steroids or immunosuppressants.
4. Treatment Resistance: As with other cancer treatments, some cancers can develop resistance to immunotherapy over time. Tumors may mutate in ways that enable them to evade immune detection or activate alternative checkpoints like LAG-3, which can inhibit the immune response (Sharma & Allison, 2015). Researchers are exploring dual checkpoint blockade therapies that target multiple checkpoint proteins simultaneously, which may help overcome resistance and improve treatment outcomes (Ribas & Wolchok, 2018).
Future Directions: The future of immunotherapy lies in personalizing treatments and developing new strategies to overcome existing challenges. Key areas of research include:
1. Personalized Treatments: Using genetic profiling and tumor-specific markers, such as neoantigens, to create tailored immunotherapies that can provide more precise and effective treatments (Sharma & Allison, 2015).
2. Bispecific Antibodies: These innovative drugs, such as blinatumomab (Blincyto®), bind to two different targets simultaneously, helping immune cells attack cancer more effectively (Rosenberg & Restifo, 2015).
3. Affordability Initiatives: Efforts to reduce costs through biosimilars, government subsidies, and international collaborations will be essential in making immunotherapy accessible to a wider population (Farkona et al., 2016).
Conclusion
Immunotherapy has revolutionized cancer treatment by providing new hope for patients with cancers that were once considered untreatable. Breakthroughs like checkpoint inhibitors and CAR T-cell therapy have demonstrated the power of using the immune system to fight cancer. However, challenges such as high costs, varying patient responses, and side effects still need to be addressed. By continuing to advance research and develop innovative solutions, immunotherapy has the potential to transform cancer care and improve outcomes for millions of patients worldwide.
References
- American Cancer Society. (2024). Cancer facts & figures 2024. https://www.cancer.org/research/cancer-facts-statistics.html
- Farkona, S., Diamandis, E. P., & Blasutig, I. M. (2016). Cancer immunotherapy: The beginning of the end of cancer? BMC Medicine, 14(1), 73. https://doi.org/10.1186/s12916-016-0623-5
- June, C. H., O’Connor, R. S., Kawalekar, O. U., Ghassemi, S., & Milone, M. C. (2018). CAR T cell immunotherapy for human cancer. Science, 359(6382), 1361–1365. https://doi.org/10.1126/science.aar6711
- Maude, S. L., Laetsch, T. W., Buechner, J., Rives, S., Boyer, M., Bittencourt, H., … & Grupp, S. A. (2018). Tisagenlecleucel in children and young adults with B-cell lymphoblastic leukemia. New England Journal of Medicine, 378(5), 439–448. https://doi.org/10.1056/NEJMoa1709866
- Ribas, A., & Wolchok, J. D. (2018). Cancer immunotherapy using checkpoint blockade. Science, 359(6382), 1350–1355. https://doi.org/10.1126/science.aar4060
- Rosenberg, S. A., & Restifo, N. P. (2015). Adoptive cell transfer as personalized immunotherapy for human cancer. Science, 348(6230), 62–68. https://doi.org/10.1126/science.aaa4967
- Schreiber, R. D., Old, L. J., & Smyth, M. J. (2011). Cancer immunoediting: Integrating immunity’s roles in cancer suppression and promotion. Science, 331(6024), 1565–1570. https://doi.org/10.1126/science.1203486
- Sharma, P., & Allison, J. P. (2015). The future of immune checkpoint therapy. Science, 348(6230), 56–61. https://doi.org/10.1126/science.aaa8172
- Topalian, S. L., Drake, C. G., & Pardoll, D. M. (2015). Immune checkpoint blockade: A common denominator approach to cancer therapy. Cancer Cell, 27(4), 450–461. https://doi.org/10.1016/j.ccell.2015.03.001